
In baPWV measurements, the brachial arterial wave is used to substitute for the proximal aortic wave. In this case, the arterial wave on the branching artery can be used instead (fig. In this case, it is not easy to apply this method, because the proximal aortic wave is difficult to measure from the body surface.
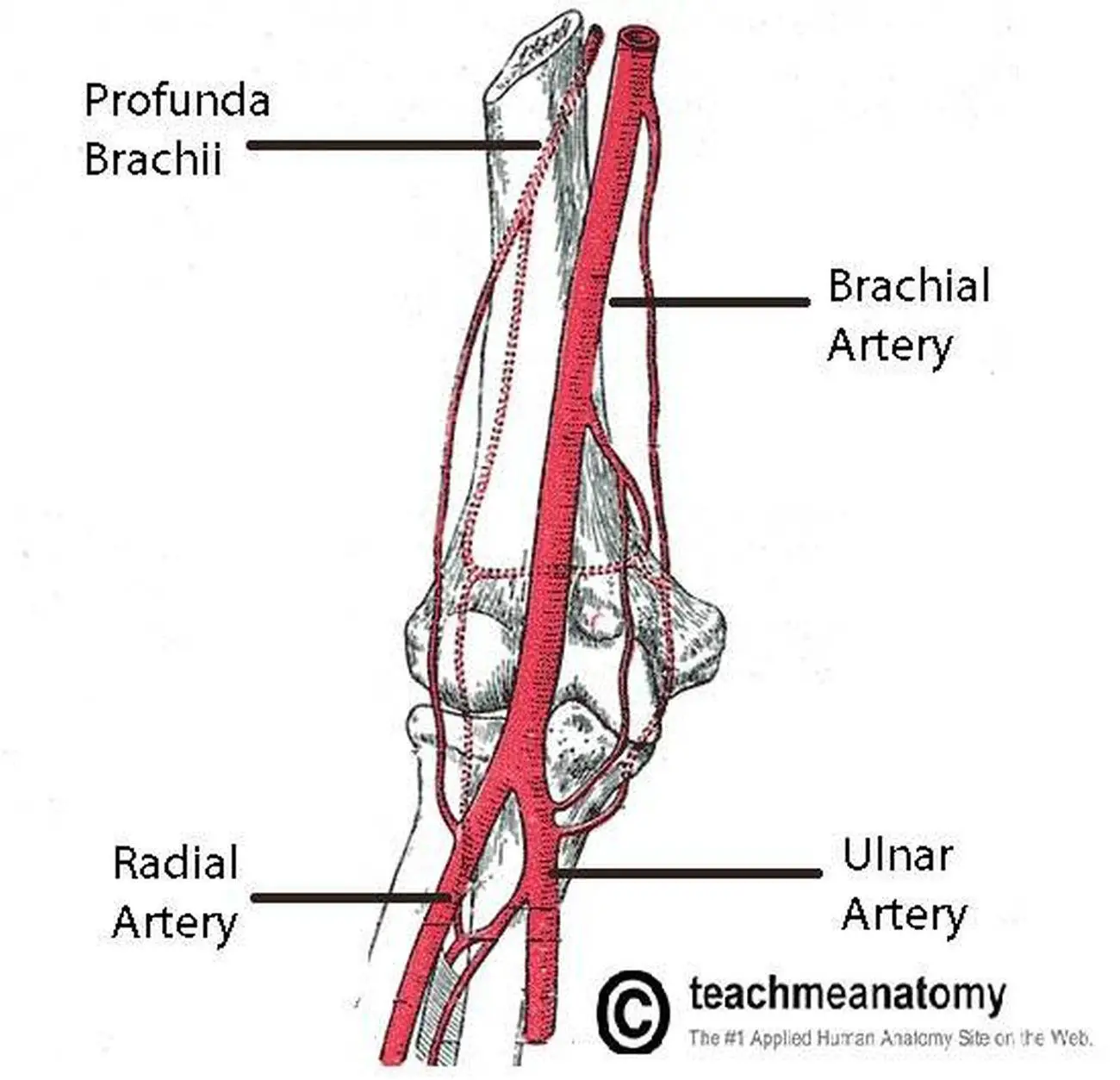
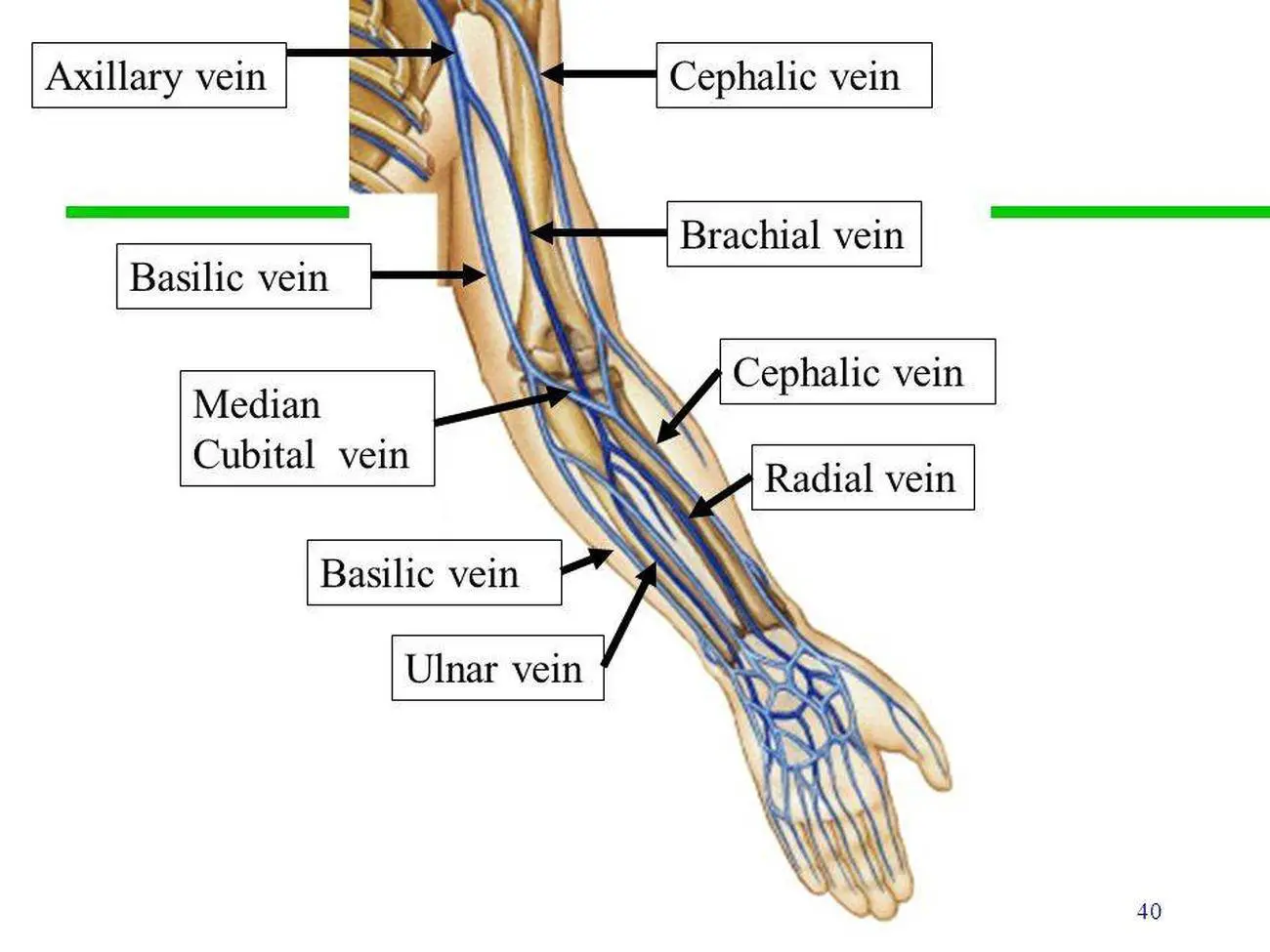
The stiffness of the large artery is considered more important than that of the peripheral artery. (fig.1a), 1a), but this can only be applied to peripheral PWV such as brachial-radial or femoral-tibial PWV. The pulse wave is preferentially measured between two points on the same artery (fig. PWV is calculated by dividing travelled distance by travel time. Theoretical Concept of baPWV and Its Validation Brachial-ankle PWV (baPWV) was developed in this historical situation in about the year 2000. In Japan, the use of these devices, however, was still limited in the research field, possibly because of their limited availability to general practitioners. Several automatic devices have been introduced for the measurement of cfPWV, and a vast amount of clinical data has been accumulated. In Western countries, carotid-femoral PWV (cfPWV) has been a popular method for evaluating large-artery stiffness, which was more importantly considered as a measure of buffering function moderating cardiac load or arterial oscillation. At the same time, analysis of finger photoplethysmographic waveforms was first introduced by Ozawa (in Japanese), and its clinical usefulness as a measure of vascular ageing was later established by Takazawa et al. In Japan, a unique technique for measuring aortic PWV was developed around 1970 and had been suggested as a marker of atherosclerosis. The PWV is known to be proportional to the rigidity of the arterial wall through which it propagates and inversely proportional to the vessel diameter. The ejection of blood from the heart produces an arterial pulsation termed ‘pulse wave’, and the speed at which it propagates to the periphery is called ‘pulse wave velocity’ (PWV). In this regard, arterial stiffness might be a good candidate. Because high blood pressure is the most important risk factor for cardiovascular diseases in the Japanese population, an arterial measure which reflects the influence of blood pressure would be an adequate marker for total vascular risk in Japanese people. Thus, arterial stiffness reflects the summation of both organic and functional stiffness of the arterial wall. Moreover, increased intraluminal pressure, or hypertension, could increase arterial wall stress and functionally stiffens the arterial wall. The arterial wall progressively stiffens because of ageing, which is associated with various kinds of biochemical and histologic changes in the arterial wall. Arterial stiffness refers to the rigidity of the arterial wall. More specifically, arterial stiffness has been considered as a measure of biological ageing. Regarding arterial health, William Osler stated: ‘Man is as old as his arteries’. Thus, healthier vascular ageing is of great concern to Japanese society. Many factors cause disability among aged Japanese individuals, but cerebrovascular diseases have been suggested to play the most important role. However, the prolongation of the life expectancy of Japanese people has not been associated with a consistently healthy life but with one with some periods of disability. In fact, systolic blood pressure values have been reduced by about 10-20 mm Hg throughout all generations during the past 50 years, resulting in a marked reduction in the incidence of stroke, a leading cause of death among Japanese until 1980.
Brachial pulse free#
This is largely attributable to the introduction of a universal health care system in 1961 and the establishment of free access to medical facilities.


The life expectancies of Japanese people have extended by about 25 years during the previous 5 decades. Ageing of society is a common issue in many developed countries.


 0 kommentar(er)
0 kommentar(er)
